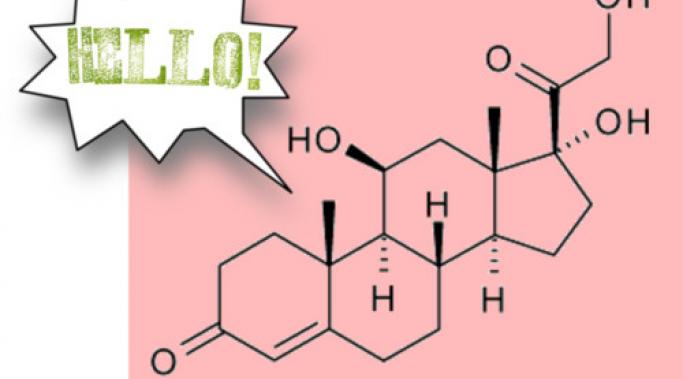
Last fall, I started reading more about cortisol, an adrenal hormone perhaps best known for its role in the fight or flight reaction. I’d heard a lot of chatter about how we’re all drenched in the stuff on account of modern life is like fighting hungry lions only without all the hungry lions. And it occurred to me that if busy work schedules and not enough down-time could produce enough excess cortisol to get medical doctors pushing things like meditation, living with trauma disorders like Dissociative Identity Disorder (DID) and Post-Traumatic Stress Disorder (PTSD) must be as dangerous as battling a pride of hungry lions on the edge of an active volcano during a hurricane.
Living with DID
When I published my last post almost a year ago, I was sure that it marked the end of Dissociative Living. I wasn’t happy about that. I was frustrated and angry with myself for what I saw as an inability to manage stress effectively. And I was sad that I had to give up writing about Dissociative Identity Disorder because of that inability. Since that post last September, I’ve learned some things, including: 1) there is a profound difference, practically speaking, between stress and chronic stress, and 2) you cannot manage chronic stress – you either survive it, or you escape it.
I'm weary. I’ve been living on the wrong side of my stress threshold for a while now. Part of the problem is that my stress threshold is maddeningly low. But part of the problem is that major things keep happening in my personal life lately; things that create enormous stress even for the most mentally healthy among us. As a result, my Dissociative Identity Disorder symptoms have amplified steadily over the last eighteen months. In the words of my fellow blogger Natasha Tracy, “When life gets nasty disease gets nasty too.” She’s right, of course. But I kept thinking, ‘hey, life is really turbulent sometimes and you just have to rise to the occasion.’ I failed to recognize, though, that doing so usually involves letting go of other, less urgent occasions.
The past few months of my life have brought with them the suicide of a family member, the substance abuse problems and sudden onset mental illness of another, some unexpected financial difficulties, and not nearly enough time and space for me to cope with it all effectively. I’ve taken the put-your-head-down-and-keep-moving approach in part because I know I’ll leave other people in the lurch if I stop to recuperate. When a tornado hits is not the time to announce that gosh, you’d love to help out but you really need some Me Time. Instead, I’ve relied on my long-held belief that Dissociative Identity Disorder is both a blessing and a curse when life gets messy. But I’ve changed my mind. All DID does is make nasty situations nastier.
I've been trying for four days now to finish an article on depersonalization, one of five primary ways dissociation manifests. I wanted to address the milder episodes of depersonalization most people experience at one time or another. But I have Dissociative Identity Disorder, and severe depersonalization is part of living with DID. Ironically enough, it's depersonalization itself - specifically, mental clouding - that's preventing me from finishing that article. I've finally decided that if I'm going to continue to try to write in a highly depersonalized state, it makes sense to stop fighting it and simply do my best to describe what I'm experiencing. The article I intended to publish today will have to wait until I can think clearly again.
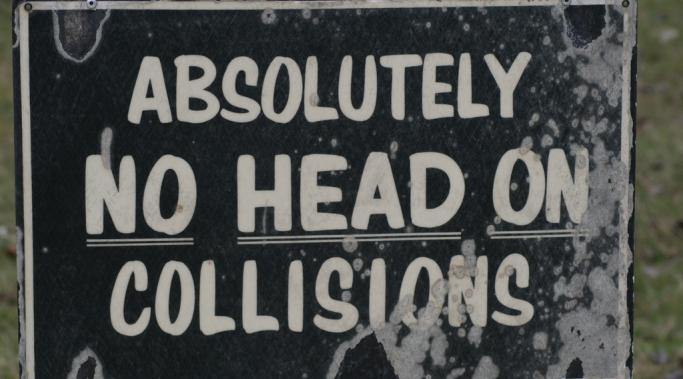
There’s a space of six weeks between my last two posts here at Dissociative Living. Some of that month and a half disappearance has to do with the fact that I’d been trying to do too much for the better part of a year and I reached a kind of critical mass that left me depleted and in desperate need of rest. And some of it has to do with the nature of Dissociative Identity Disorder itself. It’s natural, within the context of DID, to compartmentalize one’s life to such a degree that the various arenas in which we live – work, school, friends, etc. – are separate worlds altogether. And when one or more of those worlds collide, as they inevitably do from time to time, the resulting anxiety triggers a full retreat from one or all of the affected worlds. But I’ve discovered that there’s more to these disappearances than I believed.
Nothing about dissociative identity disorder is quite what the most popular phrases used to describe it imply. “Losing time” is no exception. When we talk about losing time we’re talking about severe dissociative amnesia which, in a milder form, is something I believe everyone experiences. But the phrase “losing time” suggests a highly dramatic, easily recognizable aberration. In my experience, however, dissociative amnesia is startlingly surreptitious. It’s easy to be unaware that you’re losing time at all.
I’ve discussed my difficulties with setting personal boundaries and some of what contributes to those difficulties. But it occurs to me that there may be a link between the high suggestibility of people with Dissociative Identity Disorder and the challenges so many of us face with personal boundaries. It seems reasonable that saying no would be more difficult for people who are particularly susceptible to the power of suggestion.
Like so many others with dissociative identity disorder (DID), I have comorbid posttraumatic stress disorder. But it isn’t the temporary response to short-lived trauma that most people think of as PTSD. It’s a deeper, more pervasive, and chronic response to life in general. This form of PTSD is called complex PTSD. And it occurs so often in conjunction with dissociative identity disorder, that I sometimes wonder if there's anyone with DID who doesn’t live with this monster.
Despite reminder tools and sheer determination, I keep forgetting to take my medication. I get up in the morning and think to myself, 'Now don’t forget to take your medication!' while heading to the bathroom where it’s waiting for me in a brightly colored container right there on the counter. And I repeatedly discover, much later in the day, those pills lying untouched in their little compartments. I have dissociative identity disorder and this is just one example of how my dissociative memory affects my everyday life. On its own it may not seem like a big deal. And if my memory problems were exclusive to forgetting medication or if they were irregular, here-and-there occurrences they probably wouldn’t be much of an issue. But what I just described is how my memory works all the time, with everything.