Edluar: Insomnia Medication (Full Prescribing Information)
Brand Name: Edluar
Generic Name: zolpidem tartrate
Contents:
Indications and Usage
Dosage and Administration
Dosage Forms and Strengths
Contraindications
Warnings and Precautions
Adverse Reactions
Drug Interactions
Use in Specific Populations
Drug Abuse and Dependence
Overdosage
Description
Pharmacology
Nonclinical Toxicology
Clinical Studies
How Supplied
Edluar patient information sheet (in plain English)
Indications and Usage
Edluar (zolpidem tartrate sublingual tablets) is indicated for the short-term treatment of insomnia characterized by difficulties with sleep initiation.
The clinical trials performed with Zolpidem tartrate in support of efficacy were 4-5 weeks in duration with the final formal assessments of sleep latency performed at the end of treatment (see Clinical Studies).
Dosage and Administration
The dose of Edluar should be individualized.
 Dosage in adults
Dosage in adults
The recommended dose for Edluar for adults is 10 mg once daily immediately before bedtime. The total Edluar daily dose should not exceed 10 mg.
Special Populations
Elderly or debilitated patients may be especially sensitive to the effects of zolpidem tartrate. Patients with hepatic insufficiency do not clear the drug as rapidly as normal subjects. The recommended dose of Edluar in both of these patient populations is 5 mg once daily immediately before bedtime (see Warnings and Precautions, Special Populations).
Use with CNS depressants
Dosage adjustment may be necessary when Edluar is combined with other CNS-depressant drugs because of the potentially additive effects (see Warnings and Precautions, CNS depressant effects).
Administration
The effect of Edluar may be slowed by ingestion with or immediately after a meal. Edluar should not be given with or immediately after a meal.
Edluar sublingual tablet should be placed under the tongue, where it will disintegrate. The tablet should not be swallowed and the tablet should not be taken with water.
Dosage Forms and Strengths
Edluar is available in 5 mg and 10 mg strength tablets for sublingual administration. Tablets are not scored.
Edluar 5 mg sublingual tablets are round white, flat-faced, bevel-edged, with debossed V on one side.
Edluar 10 mg sublingual tablets are round white, flat-faced, bevel-edged, with debossed X on one side.
Contraindications
Edluar is contraindicated in patients with known hypersensitivity to zolpidem tartrate or to any of the inactive ingredients in the formulation. Observed reactions include anaphylaxis and angioedema (see Warnings and Precautions, severe anaphylactic and anaphylactoid reactions and Description).
Warnings and Precautions
Need to evaluate for co-morbid diagnoses
Because sleep disturbances may be the presenting manifestation of a physical and/or psychiatric disorder, symptomatic treatment of insomnia should be initiated only after a careful evaluation of the patient. The failure of insomnia to remit after 7 to 10 days of treatment may indicate the presence of a primary psychiatric and/or medical illness that should be evaluated. Worsening of insomnia or the emergence of new thinking or behavior abnormalities may be the consequence of an unrecognized psychiatric or physical disorder. Such findings have emerged during the course of treatment with sedative/hypnotic drugs, including zolpidem tartrate.
Severe anaphylactic and anaphylactoid reactions
Rare cases of angioedema involving the tongue, glottis or larynx have been reported in patients after taking the first or subsequent doses of sedative-hypnotics, including zolpidem tartrate. Some patients have had additional symptoms such as dyspnea, throat closing or nausea and vomiting that suggest anaphylaxis. Some patients have required medical therapy in the emergency department. If angioedema involves the throat, glottis or larynx, airway obstruction may occur and be fatal. Patients who develop angioedema after treatment with Edluar should not be rechallenged with the drug.
Abnormal thinking and behavioral changes
A variety of abnormal thinking and behavior changes have been reported to occur in association with the use of sedative/hypnotics. Some of these changes may be characterized by decreased inhibition (e.g. aggressiveness and extroversion that seemed out of character), similar to effects produced by alcohol and other CNS depressants. Visual and auditory hallucinations have been reported as well as behavioral changes such as bizarre behavior, agitation and depersonalization. In controlled trials, <1% of adults with insomnia who received zolpidem tartrate reported hallucinations. In a clinical trial, 7.4% of pediatric patients with insomnia associated with attention-deficit/hyperactivity disorder (ADHD), who received zolpidem reported hallucinations (see Use in Specific Populations, pediatric use).
Complex behaviors such as "sleep-driving" (i.e., driving while not fully awake after ingestion of a sedative-hypnotic, with amnesia for the event) have been reported with sedative-hypnotics, including zolpidem tartrate. These events can occur in sedative-hypnotic-naive as well as in sedative-hypnotic-experienced persons. Although behaviors such as "sleep-driving" may occur with Edluar alone at therapeutic doses, the use of alcohol and other CNS depressants with Edluar appears to increase the risk of such behaviors, as does the use of Edluar at doses exceeding the maximum recommended dose. Due to the risk to the patient and the community, discontinuation of Edluar should be strongly considered for patients who report a "sleep-driving" episode. Other complex behaviors (e.g., preparing and eating food, making phone calls, or having sex) have been reported in patients who are not fully awake after taking a sedative-hypnotic. As with "sleep-driving", patients usually do not remember these events. Amnesia, anxiety and other neuro-psychiatric symptoms may occur unpredictably.
In primarily depressed patients, worsening of depression, including suicidal thoughts and actions (including completed suicides), has been reported in association with the use of sedative/hypnotics.
It can rarely be determined with certainty whether a particular instance of the abnormal behaviors listed above is drug-induced, spontaneous in origin, or a result of an underlying psychiatric or physical disorder. Nonetheless, the emergence of any new behavioral sign or symptom of concern requires careful and immediate evaluation.
Withdrawal effects
Following rapid dose decrease or abrupt discontinuation of sedative/hypnotics, there have been reports of signs and symptoms similar to those associated with withdrawal from other CNS-depressant drugs (see Drug Abuse and Dependence).
CNS depressant effects
Edluar, like other sedative/hypnotic drugs, has CNS-depressant effects. Due to the rapid onset of action, Edluar should be ingested immediately prior to going to bed. Patients should be cautioned against engaging in hazardous occupations requiring complete mental alertness or motor coordination such as operating machinery or driving a motor vehicle after ingesting the drug, including potential impairment of the performance of such activities that may occur the day following ingestion of Edluar. Zolpidem tartrate showed additive effects when combined with alcohol and should not be taken with alcohol. Patients should also be cautioned about possible combined effects with other CNS-depressant drugs. Dosage adjustments of Edluar may be necessary when Edluar is administered with such agents because of the potentially additive effects.
Special Populations
Use in the elderly and/or debilitated patients:
Impaired motor and/or cognitive performance after repeated exposure or unusual sensitivity to sedative/hypnotic drugs is a concern in the treatment of elderly and/or debilitated patients. Therefore, the recommended Edluar dosage is 5 mg in the elderly and/or debilitated patients (see Dosage and Administration, Special populations and Use in Specific Populations, Geriatric use) to decrease the possibility of side effects. These patients should be closely monitored.
Use in patients with concomitant illness:
Clinical experience with zolpidem tartrate in patients with concomitant systemic illness is limited. Caution is advisable in using Edluar in patients with diseases or conditions that could affect metabolism or hemodynamic responses. Although studies did not reveal respiratory depressant effects at hypnotic doses of zolpidem tartrate in normal subjects or in patients with mild to moderate chronic obstructive pulmonary disease (COPD), a reduction in the Total Arousal Index together with a reduction in lowest oxygen saturation and increase in the times of oxygen desaturation below 80% and 90% was observed in patients with mild-to-moderate sleep apnea when treated with zolpidem tartrate (10 mg) when compared to placebo. Since sedative/hypnotics have the capacity to depress respiratory drive, precautions should be taken if Edluar is prescribed to patients with compromised respiratory function. Edluar should be used with caution in patients with sleep apnea syndrome or myasthenia gravis. Post-marketing reports of respiratory insufficiency following treatment with zolpidem tartrate, most of which involved patients with pre-existing respiratory impairment, have been received.
Data in end-stage renal failure patients repeatedly treated with zolpidem tartrate did not demonstrate drug accumulation or alterations in pharmacokinetic parameters. No dosage adjustment of Edluar in renally impaired patients is required; however, these patients should be closely monitored (see Clinical Pharmacology, Pharmacokinetics).
A study in subjects with hepatic impairment treated with zolpidem tartrate did reveal prolonged elimination in this group; therefore, treatment with Edluar should be initiated with 5 mg in patients with hepatic compromise, and they should be closely monitored (see Dosage and Administration, Special populations and Clinical Pharmacology, Pharmacokinetics).
Use in patients with depression:
As with other sedative/hypnotic drugs, Edluar should be administered with caution to patients exhibiting signs or symptoms of depression. Suicidal tendencies may be present in such patients and protective measures may be required. Intentional over-dosage is more common in this group of patients; therefore, the least amount of drug that is feasible should be prescribed for the patient at any one time.
Pediatric patients:
Edluar is not recommended for use in children. Safety and effectiveness of Edluar have not been established in pediatric patients below the age of 18. In an 8-week study in pediatric patients (aged 6-17 years) with insomnia associated with ADHD, an oral solution of zolpidem did not decrease sleep latency compared to placebo. Hallucinations were reported in 7.4% of the pediatric patients who received zolpidem; none of the pediatric patients who received placebo reported hallucinations (see Use in Specific Populations, Pediatric use).
Adverse Reactions
The following serious adverse reactions are discussed in greater detail in other sections of the labeling:
- Serious anaphylactic and anaphylactoid reactions (see Warnings and Precautions, Severe anaphylactic and anaphylactoid reactions)
- Abnormal thinking and behavior, complex behaviors (see Warnings and Precautions, Abnormal thinking and behavioral changes)
- Withdrawal effects (see Warnings and Precautions, Withdrawal effects)
- CNS-depressant effects (see Warnings and Precautions, CNS depressant effects)
Clinical trials experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The adverse reaction information from clinical trials does, however, provide a basis for identifying the adverse events that appear to be related to drug use and for approximating incidence rates.
Associated with discontinuation of treatment:
Approximately 4% of 1,701 patients who received zolpidem tartrate at all doses (1.25 to 90 mg) in U.S. premarketing clinical trials discontinued treatment because of an adverse reaction. Reactions most commonly associated with discontinuation from U.S. trials were daytime drowsiness (0.5%), dizziness (0.4%), headache (0.5%), nausea (0.6%), and vomiting (0.5%).
Approximately 4% of 1,959 patients who received zolpidem tartrate at all doses (1 to 50 mg) in similar foreign trials discontinued treatment because of an adverse reaction. Reactions most commonly associated with discontinuation from these trials were daytime drowsiness (1.1%), dizziness/vertigo (0.8%), amnesia (0.5%), nausea (0.5%), headache (0.4%), and falls (0.4%).
Data from a clinical study in which selective serotonin reuptake inhibitor (SSRI)-treated patients were given zolpidem tartrate revealed that four of the seven discontinuations during double-blind treatment with zolpidem (n=95) were associated with impaired concentration, continuing or aggravated depression, and manic reaction; one patient treated with placebo (n=97) was discontinued after an attempted suicide.
Most commonly observed adverse reactions in controlled trials:
During short-term treatment (up to 10 nights) with zolpidem tartrate at doses up to 10 mg, the most commonly observed adverse reactions associated with the use of zolpidem and seen at statistically significant differences from placebo-treated patients were drowsiness (reported by 2% of zolpidem patients), dizziness (1%), and diarrhea (1%). During longer-term treatment (28 to 35 nights) with zolpidem tartrate at doses up to 10 mg, the most commonly observed adverse reactions associated with the use of zolpidem and seen at statistically significant differences from placebo-treated patients were dizziness (5%) and drugged feelings (3%).
Adverse reactions observed at an incidence of ≥1% in controlled trials:
The following tables enumerate treatment-emergent adverse event frequencies that were observed at an incidence equal to 1% or greater among patients with insomnia who received zolpidem tartrate and at a greater incidence than placebo in U.S. placebo-controlled trials. Events reported by investigators were classified utilizing a modified World Health Organization (WHO) dictionary of preferred terms for the purpose of establishing event frequencies. The prescriber should be aware that these figures cannot be used to predict the incidence of side effects in the course of usual medical practice, in which patient characteristics and other factors differ from those that prevailed in these clinical trials. Similarly, the cited frequencies cannot be compared with figures obtained from other clinical investigators involving related drug products and uses, since each group of drug trials is conducted under a different set of conditions. However, the cited figures provide the physician with a basis for estimating the relative contribution of drug and nondrug factors to the incidence of side effects in the population studied.
The following table was derived from a pool of 11 placebo-controlled short-term U.S. efficacy trials involving zolpidem in doses ranging from 1.25 to 20 mg. The table is limited to data from doses up to and including 10 mg, the highest dose recommended for use.
| *Reactions reported by at least 1% of patients treated with oral zolpidem and at a greater frequency than placebo. | ||
| Body System/ Adverse Event* |
Zolipidem tartrate (≤ 10 mg) (N=685) |
Placebo (N=473) |
| Central and Peripheral Nervous System | ||
| Headache | 7 | 6 |
| Drowsiness | 2 | - |
| Dizziness | 1 | - |
| Gastrointestinal System | ||
| Diarrhea | 1 | |
The following table was derived from a pool of three placebo-controlled long-term efficacy trials involving oral zolpidem. These trials involved patients with chronic insomnia who were treated for 28 to 35 nights with zolpidem at doses of 5, 10, or 15 mg. The table is limited to data from doses up to and including 10 mg, the highest dose recommended for use. The table includes only adverse events occurring at an incidence of at least 1% for zolpidem patients.
| *Reactions reported by at least 1% of patients treated with oral zolpidem and at a greater frequency than placebo. | ||
| Body System/ Adverse Event* |
Zolpidem tartrate (≤ 10 mg) (N=152) |
Placebo (N=161) |
| Autonomic Nervous System | 3 | 1 |
| Dry mouth | ||
Body as a Whole |
||
| Allergy | 4 | 1 |
| Back Pain | 3 | 2 |
| Influenza-like symptoms | 2 | - |
| Chest pain | 1 | - |
Cardiovascular System |
||
| Palpitation | 2 | - |
Central and Peripheral Nervous System |
||
| Drowsiness | 8 | 5 |
| Dizziness | 5 | 1 |
| Lethargy | 3 | 1 |
| Drugged feeling | 3 | - |
| Lightheadedness | 2 | 1 |
| Depression | 2 | 1 |
| Abnormal dreams | 1 | - |
| Amnesia | 1 | - |
| Sleep disorder | 1 | - |
Gastrointestinal System |
||
| Diarrhea | 3 | 2 |
| Abdominal pain | 2 | 2 |
| Constipation | 2 | 1 |
Respiratory System |
||
| Sinusitis | 4 | 2 |
| Pharyngitis | 3 | 1 |
Skin and Appendages |
||
| Rash | 2 | 1 |
Dose relationship for adverse reactions associated with oral zolpidem:
There is evidence from dose comparison trials suggesting a dose relationship for many of the adverse reactions associated with oral zolpidem use, particularly for certain CNS and gastrointestinal adverse events.
Oral tissue-related adverse reactions to Edluar:
The effect of chronic daily administration of Edluar on oral tissue was evaluated in a 60-day open-label study in 60 insomniac patients. One patient developed transient sublingual erythema, and another transient paresthesia of the tongue.
Adverse event incidence across the entire preapproval oral zolpidem database:
Zolpidem was administered to 3,660 subjects in clinical trials throughout the U.S., Canada, and Europe. Treatment-emergent adverse events associated with clinical trial participation were recorded by clinical investigators using terminology of their own choosing. To provide a meaningful estimate of the proportion of individuals experiencing treatment-emergent adverse events, similar types of untoward events were grouped into a smaller number of standardized event categories and classified utilizing a modified World Health Organization (WHO) dictionary of preferred terms.
The frequencies presented, therefore, represent the proportions of the 3,660 individuals exposed to zolpidem, at all doses, who experienced an event of the type cited on at least one occasion while receiving zolpidem. All reported treatment-emergent adverse events are included, except those already listed in the table above of adverse events in placebo-controlled studies, those coding terms that are so general as to be uninformative, and those events where a drug cause was remote. It is important to emphasize that, although the events reported did occur during treatment with zolpidem, they were not necessarily caused by it.
Adverse events are further classified within body system categories and enumerated in order of decreasing frequency using the following definitions: frequent adverse events are defined as those occurring in greater than 1/100 subjects; infrequent adverse events are those occurring in 1/100 to 1/1,000 patients; rare events are those occurring in less than 1/1,000 patients.
Autonomic nervous system: Infrequent: increased sweating, pallor, postural hypotension, syncope. Rare: abnormal accommodation, altered saliva, flushing, glaucoma, hypotension, impotence, increased saliva, tenesmus.
Body as a whole: Frequent: asthenia. Infrequent: edema, falling, fever, malaise, trauma. Rare: allergic reaction, allergy aggravated, anaphylactic shock, face edema, hot flashes, increased ESR, pain, restless legs, rigors, tolerance increased, weight decrease.
Cardiovascular system: Infrequent: cerebrovascular disorder, hypertension, tachycardia. Rare: angina pectoris, arrhythmia, arteritis, circulatory failure, extrasystoles, hypertension aggravated, myocardial infarction, phlebitis, pulmonary embolism, pulmonary edema, varicose veins, ventricular tachycardia.
Central and peripheral nervous system: Frequent: ataxia, confusion, euphoria, headache, insomnia, vertigo. Infrequent: agitation, anxiety, decreased cognition, detached, difficulty concentrating, dysarthria, emotional lability, hallucination, hypoesthesia, illusion, leg cramps, migraine, nervousness, paresthesia, sleeping (after daytime dosing), speech disorder, stupor, tremor. Rare: abnormal gait, abnormal thinking, aggressive reaction, apathy, appetite increased, decreased libido, delusion, dementia, depersonalization, dysphasia, feeling strange, hypokinesia, hypotonia, hysteria, intoxicated feeling, manic reaction, neuralgia, neuritis, neuropathy, neurosis, panic attacks, paresis, personality disorder, somnambulism, suicide attempts, tetany, yawning.
Gastrointestinal system: Frequent: dyspepsia, hiccup, nausea. Infrequent: anorexia, constipation, dysphagia, flatulence, gastroenteritis, vomiting. Rare: enteritis, eructation, esophagospasm, gastritis, hemorrhoids, intestinal obstruction, rectal hemorrhage, tooth caries.
Hematologic and lymphatic system: Rare: anemia, hyperhemoglobinemia, leukopenia, lymphadenopathy, macrocytic anemia, purpura, thrombosis.
Immunologic system: Infrequent: infection. Rare: abscess herpes simplex herpes zoster, otitis externa, otitis media.
Liver and biliary system: Infrequent: abnormal hepatic function, increased SGPT. Rare: bilirubinemia, increased SGOT.
Metabolic and nutritional: Infrequent: hyperglycemia, thirst. Rare: gout, hypercholesteremia, hyperlipidemia, increased alkaline phosphatase, increased BUN, periorbital edema.
Musculoskeletal system: Frequent: arthralgia, myalgia. Infrequent: arthritis. Rare: arthrosis, muscle weakness, sciatica, tendinitis.
Reproductive system: Infrequent: menstrual disorder, vaginitis. Rare: breast fibroadenosis, breast neoplasm, breast pain.
Respiratory system: Frequent: upper respiratory infection. Infrequent: bronchitis, coughing, dyspnea, rhinitis. Rare: bronchospasm, epistaxis, hypoxia, laryngitis, pneumonia.
Skin and appendages: Infrequent: pruritus. Rare: acne, bullous eruption, dermatitis, furunculosis, injection-site inflammation, photosensitivity reaction, urticaria.
Special senses: Frequent: diplopia, vision abnormal. Infrequent: eye irritation, eye pain, scleritis, taste perversion, tinnitus. Rare: conjunctivitis, corneal ulceration, lacrimation abnormal, parosmia, photopsia.
Urogenital system: Infrequent: urinary tract infection. Infrequent: cystitis, urinary incontinence. Rare: acute renal failure, dysuria, micturition frequency, nocturia, polyuria, pyelonephritis, renal pain, urinary retention.
Drug Interactions
For details of drug interactions, please refer to (Clinical Pharmacology, Pharmacokinetics).
CNS-active drugs
Any drug with CNS-depressant effects could potentially enhance the CNS-depressant effects of zolpidem.
Imipramine in combination with zolpidem produced an additive effect of decreased alertness. Similarly, chlorpromazine in combination with zolpidem produced an additive effect of decreased alertness and psychomotor performance. These drugs did not show any significant pharmacokinetic interaction.
A study involving haloperidol and zolpidem revealed no effect of haloperidol on the pharmacokinetics or pharmacodynamics of zolpidem. The lack of a drug interaction following single-dose administration does not predict a lack following chronic administration.
An additive effect on psychomotor performance between alcohol and oral zolpidem was demonstrated (see Warnings and Precautions: CNS depressant effects). Concomitant administration of zolpidem and sertraline increased zolpidem Cmax (43%) and decreased Tmax (53%), whether or not these changes alter the pharmacodynamic effect of zolpidem is unknown.
Drugs that affect drug metabolism via cytochrome P450
Some compounds known to inhibit CYP3A may increase exposure to zolpidem. The effect of inhibitors of other P450 enzymes has not been carefully evaluated.
Co-administration of multiple doses of rifampin and a single dose of zolpidem tartrate (20 mg) given 17 hours after the last dose of rifampin showed significant reductions of the AUC (73%), Cmax (58%), and T1/2 (36%) of zolpidem together with significant reductions in the pharmacodynamic effects of zolpidem tartrate.
Co-administration of a single dose of zolpidem tartrate with 4 doses of ketoconazole, a potent CYP3A4 inhibitor increased Cmax of zolpidem (30%) and the total AUC of zolpidem (70%) compared to zolpidem alone and prolonged the elimination half-life (30%) along with an increase in the pharmacodynamic effects of zolpidem. Consideration should be given to using a lower dose of zolpidem when ketoconazole and zolpidem are given together. Patients should be advised that use of Edluar with ketoconazole may enhance the sedative effects.
Drug-laboratory test interactions
Zolpidem is not known to interfere with commonly employed clinical laboratory tests. In addition, clinical data indicate that zolpidem does not cross-react with benzodiazepines, opiates, barbiturates, cocaine, cannabinoids, or amphetamines in two standard urine drug screens.
Use in Specific Populations
Pregnancy
Pregnancy Category C:
There are no adequate and well-controlled studies of Edluar in pregnant women. Edluar should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Studies to assess the effects on children whose mothers took zolpidem during pregnancy have not been conducted. There is a published case report documenting the presence of zolpidem in human umbilical cord blood. Children born to mothers taking sedative-hypnotic drugs may be at some risk for withdrawal symptoms from the drug during the postnatal period. In addition, neonatal flaccidity has been reported in infants born to mothers who received sedative-hypnotic drugs during pregnancy.
Administration of zolpidem to pregnant rats and rabbits resulted in adverse effects on offspring development at doses greater than the maximum recommended human dose (MRHD) of 10 mg/day (8 mg/day zolpidem base); however, teratogenicity was not observed.
When zolpidem was administered at oral doses of 4, 20, and 100 mg base/kg (approximately 5, 24, and 120 times the MRHD on a mg/m2 basis) to pregnant rats during the period of organogenesis, dose-related decreases in fetal skull ossification occurred at all but the lowest dose, which is approximately 5 times the MRHD on a mg/m2 basis. In rabbits treated during organogenesis with zolpidem at oral doses of 1, 4, and 16 mg base/kg (approximately 2.5, 10, and 40 times the MRHD on a mg/m2 basis), increased embryo-fetal death and incomplete fetal skeletal ossification occurred at the highest dose. The no-effect dose for embryo-fetal toxicity in rabbits is approximately 10 times the MRHD on a mg/m2 basis. Administration of zolpidem to rats at oral doses of 4, 20, and 100 mg base/kg (approximately 5, 24, and 120 times the MRHD on a mg/m2 basis) during the latter part of pregnancy and throughout lactation produced decreased offspring growth and survival at all but the lowest dose, which is approximately 5 times the MRHD on a mg/m2 basis.
Labor and delivery
Edluar has no established use in labor and delivery (see Use in Specific Populations, Pregnancy).
Nursing mothers
Zolpidem is excreted into human milk. Studies in lactating mothers indicate that the T1/2 of zolpidem is similar to that in non-lactating women (2.6 ± 0.3 hours). The effect of zolpidem on the nursing infant is not known. Caution should be exercised when Edluar is administered to a nursing mother.
Pediatric use
Safety and effectiveness of Edluar have not been established in pediatric patients below the age of 18.
In an 8-week controlled study, 201 pediatric patients (aged 6-17 years) with insomnia associated with attention-deficit/hyperactivity disorder (90% of the patients were using psychoanaleptics) were treated with an oral solution of zolpidem (n=136), or placebo (n=65). Zolpidem did not significantly decrease latency to persistent sleep, compared to placebo, as measured by polysomnography after 4 weeks of treatment. Psychiatric and nervous system disorders comprised the most frequent (>5%) treatment-emergent adverse reactions observed with zolpidem versus placebo and included dizziness (23.5% vs. 1.5%), headache (12.5% vs. 9.2%), and hallucinations (7.4% vs. 0%) (see Warnings and Precautions, Special populations). Ten patients on zolpidem (7.4%) discontinued treatment due to an adverse reaction.
Geriatric use
A total of 154 patients in U.S. controlled clinical trials and 897 patients in non-U.S. clinical trials who received oral zolpidem were ≥60 years of age. For a pool of U.S. patients receiving zolpidem tartrate at doses of ≤10 mg or placebo, there were three adverse events occurring at an incidence of at least 3% for zolpidem and for which the zolpidem incidence was at least twice the placebo incidence (i.e., they could be considered drug-related).
| Adverse Event | Zolpidem | Placebo |
| Dizziness | 3% | 0% |
| Drowsiness | 5% | 2% |
| Diarrhea | 3% | 1% |
A total of 30/1,959 (1.5%) non-U.S. patients receiving zolpidem tartrate reported falls, including 28/30 (93%) who were ≥70 years of age. Of these 28 patients, 23 (82%) were receiving zolpidem doses >10 mg. A total of 24/1,959 (1.2%) non-U.S. patients receiving zolpidem reported confusion, including 18/24 (75%) who were ≥70 years of age. Of these 18 patients, 14 (78%) were receiving zolpidem doses >10 mg.
The dose of Edluar in elderly patients is 5 mg to minimize adverse effects related to impaired motor and/or cognitive performance and unusual sensitivity to sedative/hypnotic drugs (see Dosage and Administration, Warnings and Precautions, Clinical Pharmacology and Clinical Studies).
Drug Abuse and Dependence
Controlled substance
Edluar contains the same active substance, zolpidem tartrate, as zolpidem tartrate oral tablets and is classified as a Schedule IV controlled substance by federal regulation.
Abuse
Abuse and addiction are separate and distinct from physical dependence and tolerance. Abuse is characterized by misuse of the drug for non-medical purposes, often in combination with other psychoactive substances. Tolerance is a state of adaptation in which exposure to a drug induces changes that result in a diminution of one or more of the drug effects over time. Tolerance may occur to both desired and undesired effects of drugs and may develop at different rates for different effects.
Addiction is a primary, chronic, neurobiological disease with genetic, psychosocial, and environmental factors influencing its development and manifestations. It is characterized by behaviors that include one or more of the following: impaired control over drug use, compulsive use, continued use despite harm, and craving. Drug addiction is a treatable disease, using a multidisciplinary approach, but relapse is common.
Studies of abuse potential in former drug abusers found that the effects of single doses of zolpidem tartrate 40 mg were similar, but not identical, to diazepam 20 mg, while zolpidem tartrate 10 mg was difficult to distinguish from placebo.
Because persons with a history of addiction to, or abuse of, drugs or alcohol are at increased risk for misuse, abuse, and addiction of Edluar, they should be monitored carefully when receiving Edluar or any other hypnotic.
Dependence
Physical dependence is a state of adaptation that is manifested by a specific withdrawal syndrome that can be produced by abrupt cessation, rapid dose reduction, decreasing blood level of the drug, and/or administration of an antagonist.
Sedative/hypnotics have produced withdrawal signs and symptoms following abrupt discontinuation. These reported symptoms range from mild dysphoria and insomnia to a withdrawal syndrome that may include abdominal and muscle cramps, vomiting, sweating, tremors, and convulsions. The following adverse events which are considered to meet the DSM-III-R criteria for uncomplicated sedative/hypnotic withdrawal were reported during U.S. clinical trials following placebo substitution occurring within 48 hours following last zolpidem tartrate treatment: fatigue, nausea, flushing, lightheadedness, uncontrolled crying, emesis, stomach cramps, panic attack, nervousness, and abdominal discomfort. These reported adverse events occurred at an incidence of 1% or less. However, available data cannot provide a reliable estimate of the incidence, if any, of dependence during treatment at recommended doses. Post-marketing reports of abuse, dependence and withdrawal have been received.
Overdosage
Signs and symptoms
In postmarketing experience of overdose with zolpidem tartrate alone, or in combination with CNS-depressant agents, impairment of consciousness ranging from somnolence to coma, cardiovascular and/or respiratory compromise, and fatal outcomes have been reported.
Recommended treatment
Based on data obtained for zolpidem tartrate, general symptomatic and supportive measures for overdose with Edluar should be used along with immediate gastric lavage where appropriate. Intravenous fluids should be administered as needed. Zolpidem's sedative/hypnotic effect was shown to be reduced by flumazenil and therefore may be useful; however, flumazenil administration may contribute to the appearance of neurological symptoms (convulsions). As in all cases of drug overdose, respiration, pulse, blood pressure, and other appropriate signs should be monitored and general supportive measures employed. Hypotension and CNS depression should be monitored and treated by appropriate medical intervention. Sedating drugs should be withheld following zolpidem overdosage, even if excitation occurs. The value of dialysis in the treatment of overdosage has not been determined, although hemodialysis studies in patients with renal failure receiving therapeutic doses have demonstrated that zolpidem is not dialyzable.
As with the management of all overdosage, the possibility of multiple drug ingestion should be considered. The physician may wish to consider contacting a poison control center for up-to-date information on the management of hypnotic drug product overdosage.
Description
Edluar (zolpidem tartrate sublingual tablet) is a non-benzodiazepine hypnotic of the imidazopyridine class and is available in 5 mg and 10 mg strength tablets for sublingual administration.
Chemically, zolpidem tartrate is N,N,6-trimethyl-2-p-tolylimidazo[1,2-a] pyridine-3-acetamide L-(+)-tartrate (2:1). It has the following structure:
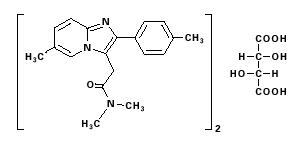
Zolpidem tartrate is a white to off-white crystalline powder that is sparingly soluble in water, alcohol, and propylene glycol. It has a molecular weight of 764.88.
Each Edluar tablet includes the following inactive ingredients: mannitol, colloidal silicon dioxide, silicified microcrystalline cellulose, croscarmellose sodium, saccharin sodium, and magnesium stearate.
Clinical Pharmacology
Mechanism of action
Zolpidem, the active moiety of zolpidem tartrate, is a hypnotic agent with a chemical structure unrelated to benzodiazepines, barbiturates, or other drugs with known hypnotic properties. It interacts with a GABA-BZ receptor complex and shares some of the pharmacological properties of the benzodiazepines. In contrast to the benzodiazepines, which non-selectively bind to and activate all BZ receptor subtypes, zolpidem in vitro binds the BZ1 receptor preferentially with a high affinity ratio of the α1/α5 subunits. This selective binding of zolpidem on the BZ1 receptor is not absolute, but it may explain the relative absence of myorelaxant and anticonvulsant effects in animal studies as well as the preservation of deep sleep (stages 3 and 4) in human studies of zolpidem tartrate at hypnotic doses.
Pharmacokinetics
Absorption:
Edluar is bioequivalent to Ambien® tablets (Sanofi-Aventis) with respect to Cmax and AUC. Similar to zolpidem tartrate oral tablets, Edluar sublingual tablets result in a pharmacokinetic profile characterized by rapid absorption.
Following administration of single 10 mg Edluar, in 18 (18-65 years of age) healthy adult subjects, the mean peak concentration (Cmax) of zolpidem was 106 ng/mL (range: 52 to 205 ng/ml) occurring at a median time (Tmax) of 82 minutes (range: 30-180 min).
A food-effect study in 18 healthy volunteers compared the pharmacokinetics of Edluar 10 mg when administered while fasting or within 20 minutes after a high fat meal. The mean AUC and Cmax were decreased by 20% and 31%, respectively, while median Tmax was prolonged by 28% (from 82 to 105 min). The half-life remained unchanged. These results suggest that, for faster sleep onset, Edluar should not be administered with or immediately after a meal.
Distribution:
Based on data obtained with oral zolpidem, the total protein binding was found to be 92.5 ± 0.1% and remained constant, independent of concentration between 40 and 790 ng/mL.
Metabolism:
Based on data obtained with oral zolpidem, zolpidem is converted to inactive metabolites that are eliminated primarily by renal excretion.
Elimination:
When Edluar administered as a single 5 or 10 mg dose in healthy adult subjects, the mean zolpidem elimination half-life was 2.85 hours (range: 1.57-6.73 hr) and 2.65 hours (range: 1.75 to 3.77 hr) respectively.
Special Populations
Elderly:
In the elderly, the dose for Edluar should be 5 mg (see Warnings and Precautions and Dosage and Administration). This recommendation is based on several studies with zolpidem tartrate in which the mean Cmax, T1/2, and AUC were significantly increased when compared to results in young adults. In one study of eight elderly subjects (>70 years), the means for Cmax, T1/2, and AUC significantly increased by 50% (255 vs. 384 ng/mL), 32% (2.2 vs. 2.9 hr), and 64% (955 vs. 1,562 ng-hr/mL), respectively, as compared to younger adults (20 to 40 years) following a single 20 mg oral dose. Zolpidem did not accumulate in elderly subjects following nightly oral dosing of 10 mg for 1 week.
Hepatic Impairment:
The pharmacokinetics of zolpidem tartrate in eight patients with chronic hepatic insufficiency were compared to results in healthy subjects. Following a single 20-mg oral zolpidem tartrate dose, mean Cmax and AUC were found to be two times (250 vs. 499 ng/mL) and five times (788 vs. 4,203 ng-hr/mL) higher, respectively, in hepatically-compromised patients. Tmax did not change. The mean half-life in cirrhotic patients of 9.9 hr (range: 4.1 to 25.8 hr) was greater than that observed in normals of 2.2 hr (range: 1.6 to 2.4 hr). Dosing with Edluar should be modified accordingly in patients with hepatic insufficiency (see Dosage and Administration, Special populations and Warnings and Precautions, Special populations).
Renal Impairment:
The pharmacokinetics of zolpidem tartrate were studied in 11 patients with end-stage 4 renal failure (mean ClCr = 6.5 ± 1.5 mL/min) undergoing hemodialysis three times a week, who were dosed with zolpidem tartrate 10 mg orally each day for 14 or 21 days. No statistically significant differences were observed for Cmax, Tmax, half-life, and AUC between the first and last day of drug administration when baseline concentration adjustments were made. On day 1, Cmax was 172 ± 29 ng/mL (range: 46 to 344 ng/mL). After repeated dosing for 14 or 21 days, Cmax was 203 ± 32 ng/mL (range: 28 to 316 ng/mL). On day 1, Tmax was 1.7 ± 0.3 hr (range: 0.5 to 3.0 hr); after repeated dosing Tmax was 0.8 ± 0.2 hr (range: 0.5 to 2.0 hr). This variation is accounted for by noting that last-day serum sampling began 10 hours after the previous dose, rather than after 24 hours. This resulted in residual drug concentration and a shorter period to reach maximal serum concentration. On day 1, T1/2 was 2.4 ± 0.4 hr (range: 0.4 to 5.1 hr). After repeated dosing, T1/2 was 2.5 ± 0.4 hr (range: 0.7 to 4.2 hr). AUC was 796 ± 159 ng-hr/mL after the first dose and 818 ± 170 ng-hr/mL after repeated dosing. Zolpidem was not hemodialyzable. No accumulation of unchanged drug appeared after 14 or 21 days. Zolpidem pharmacokinetics were not significantly different in renally-impaired patients. No dosage adjustment of Edluar is necessary in patients with compromised renal function.
Drug Interactions
CNS-active drugs:
Since the systematic evaluations of zolpidem in combination with other CNS-active drugs have been limited, careful consideration should be given to the pharmacology of any CNS-active drug to be used with zolpidem. Any drug with CNS-depressant effects could potentially enhance the CNS-depressant effects of zolpidem.
Zolpidem tartrate was evaluated in healthy volunteers in single-dose interaction studies for several CNS drugs. Imipramine in combination with zolpidem produced no pharmacokinetic interaction other than a 20% decrease in peak levels of imipramine, but there was an additive effect of decreased alertness. Similarly, chlorpromazine in combination with zolpidem produced no pharmacokinetic interaction, but there was an additive effect of decreased alertness and psychomotor performance.
A study involving haloperidol and zolpidem revealed no effect of haloperidol on the pharmacokinetics or pharmacodynamics of zolpidem. The lack of a drug interaction following single-dose administration does not predict a lack following chronic administration.
An additive effect on psychomotor performance between alcohol and oral zolpidem was demonstrated (see Warnings and Precautions,: CNS depressant effects).
A single-dose interaction study with zolpidem tartrate10 mg and fluoxetine 20 mg at steady-state levels in male volunteers did not demonstrate any clinically significant pharmacokinetic or pharmacodynamic interactions. When multiple doses of zolpidem and fluoxetine at steady state the concentrations were evaluated in healthy females, increase in the zolpidem half-life (17%) was observed. There was no evidence of an additive effect in psychomotor performance.
Following five consecutive nightly doses of oral zolpidem tartrate10 mg in the presence of sertraline 50 mg (17 consecutive daily doses, at 7:00 am, in healthy female volunteers), zolpidem Cmax was significantly higher (43%) and Tmax was significantly decreased (53%). Pharmacokinetics of sertraline and N-desmethylsertraline were unaffected by zolpidem.
Drugs that affect drug metabolism via cytochrome P450:
Some compounds known to inhibit CYP3A may increase exposure to zolpidem. The effect of inhibitors of other P450 enzymes has not been carefully evaluated.
A randomized, double-blind, crossover interaction study in ten healthy volunteers between itraconazole (200 mg once daily for 4 days) and a single dose of zolpidem tartrate (10 mg) given 5 hours after the last dose of itraconazole resulted in a 34% increase in AUC0-β of zolpidem tartrate. There were no significant pharmacodynamic effects of zolpidem on subjective drowsiness, postural sway, or psychomotor performance.
A randomized, placebo-controlled, crossover interaction study in eight healthy female subjects between five consecutive daily doses of rifampin (600 mg) and a single dose of zolpidem tartrate (20 mg) given 17 hours after the last dose of rifampin showed significant reductions of the AUC (73%), Cmax (58%), and T1/2 (36 %) of zolpidem together with significant reductions in the pharmacodynamic effects of zolpidem tartrate.
A randomized double-blind crossover interaction study in twelve healthy subjects showed that co-administration of a single 5 mg dose of zolpidem tartrate with ketoconazole, a potent CYP3A4 inhibitor, given as 200 mg twice daily for 2 days increased Cmax of zolpidem (30%) and the total AUC of zolpidem (70%) compared to zolpidem alone and prolonged the elimination half-life (30 %) along with an increase in the pharmacodynamic effects of zolpidem. Consideration should be given to using a lower dose of zolpidem when ketoconazole and zolpidem are given together. Patients should be advised that use of Edluar with ketoconazole may enhance the sedative effects.
Other drugs with no interactions with zolpidem:
A study involving cimetidine/zolpidem tartrate and ranitidine/zolpidem tartrate combinations revealed no effect of either drug on the pharmacokinetics or pharmacodynamics of zolpidem.
Zolpidem tartrate had no effect on digoxin pharmacokinetics and did not affect prothrombin time when given with warfarin in normal subjects.
Nonclinical Toxicology
Carcinogenesis, mutagenesis, impairment of fertility
Carcinogenesis:
Zolpidem was administered to mice and rats for 2 years at dietary dosages of 4, 18, and 80 mg base/kg. In mice, these doses are ≈2.5, 10, and 50 times the maximum recommended human dose (MRHD) of 10 mg/day (8 mg zolpidem base) on mg/m2 basis. In rats, these doses are ≈5, 20, and 100 times the MRHD on a mg/m2 basis. No evidence of carcinogenic potential was observed in mice. In rats, renal tumors (lipoma, liposarcoma) were seen at the mid- and high doses.
Mutagenesis:
Zolpidem was negative in in vitro (bacterial reverse mutation, mouse lymphoma, and chromosomal aberration) and in vivo (mouse micronucleus) genetic toxicology assays.
Impairment of fertility:
Oral administration of zolpidem (doses of 4, 20, and 100 mg base/kg or ≈5, 24, and 120 times the MRHD on a mg/m2 basis) to rats prior to and during mating, and continuing in females through postpartum day 25, resulted in irregular estrus cycles and prolonged precoital intervals. The no-effect dose for these findings is ≈24 times the MRHD on a mg/m2 basis. There was no impairment of fertility at any dose tested.
Clinical Studies
Chronic insomnia
Zolpidem was evaluated in two controlled studies for the treatment of patients with chronic insomnia (most closely resembling primary insomnia, as defined in the APA Diagnostic and Statistical Manual of Mental Disorders, DSM-IV™). Adult outpatients with chronic insomnia (n = 75) were evaluated in a double-blind, parallel group, 5-week trial comparing two doses of zolpidem tartrate and placebo. On objective (polysomnographic) measures of sleep latency and sleep efficiency, zolpidem 10 mg was superior to placebo on sleep latency for the first 4 weeks and on sleep efficiency for weeks 2 and 4. Zolpidem was comparable to placebo on number of awakenings at both doses studied.
Adult outpatients (n=141) with chronic insomnia were also evaluated, in a double-blind, parallel group, 4-week trial comparing two doses of zolpidem and placebo. Zolpidem 10 mg was superior to placebo on a subjective measure of sleep latency for all 4 weeks, and on subjective measures of total sleep time, number of awakenings, and sleep quality for the first treatment week.
Increased wakefulness during the last third of the night as measured by polysomnography has not been observed in clinical trials with zolpidem tartrate.
Transient insomnia
Normal adults experiencing transient insomnia (n = 462) during the first night in a sleep laboratory were evaluated in a double-blind, parallel group, single-night trial comparing two doses of zolpidem tartrate oral tablets (7.5 and 10 mg) and placebo. Both zolpidem doses were superior to placebo on objective (polysomnographic) measures of sleep latency, sleep duration, and number of awakenings.
Normal elderly adults (mean age 68) experiencing transient insomnia (n = 35) during the first two nights in a sleep laboratory were evaluated in a double-blind, crossover, 2-night trial comparing four doses of zolpidem (5, 10, 15 and 20 mg) and placebo. All zolpidem doses were superior to placebo on the two primary PSG parameters (sleep latency and efficiency) and all four subjective outcome measures (sleep duration, sleep latency, number of awakenings, and sleep quality).
Studies pertinent to safety concerns for sedative/hypnotic drugs
Next-day residual effects:
Next-day residual effects of zolpidem tartrate were evaluated in seven studies involving normal subjects. In three studies in adults (including one study in a phase advance model of transient insomnia) and in one study in elderly subjects, a small but statistically significant decrease in performance was observed in the Digit Symbol Substitution Test (DSST) when compared to placebo. Studies of zolpidem tartrate in non-elderly patients with insomnia did not detect evidence of next-day residual effects using the DSST, the Multiple Sleep Latency Test (MSLT), and patient ratings of alertness.
Rebound effects:
There was no objective (polysomnographic) evidence of rebound insomnia at recommended doses seen in studies evaluating sleep on the nights following discontinuation of zolpidem tartrate. There was subjective evidence of impaired sleep in the elderly on the first post-treatment night at doses of zolpidem tartrate above the recommended elderly dose of 5 mg.
Memory impairment:
Controlled studies in adults utilizing objective measures of memory yielded no consistent evidence of next-day memory impairment following the administration of zolpidem tartrate. However, in one study involving zolpidem doses of 10 and 20 mg, there was a significant decrease in next-morning recall of information presented to subjects during peak drug effect (90 minutes post-dose), i.e., these subjects experienced anterograde amnesia. There was also subjective evidence from adverse event data for anterograde amnesia occurring in association with the administration of zolpidem tartrate, predominantly at doses above 10 mg.
Effects on sleep stages:
In studies that measured the percentage of sleep time spent in each sleep stage, zolpidem tartrate has generally been shown to preserve sleep stages. Sleep time spent in stages 3 and 4 (deep sleep) was found comparable to placebo with only inconsistent, minor changes in REM (paradoxical) sleep at the recommended dose.
How Supplied
Edluar is supplied as sublingual tablets in two dosage strengths: Tablets are not scored.
Edluar 5 mg sublingual tablets are round white tablets, flat-faced, bevel-edged with debossed V on one side and supplied as:
NDC Number Size
0037 - 6050 - 30 blister pack of 30
The blister packs consist of aluminum/aluminum Child Resistant Control (CRC) blisters.
Edluar 10 mg sublingual tablets are round white tablets, flat-faced, bevel-edged with debossed X on one side and supplied as:
NDC Number Size
0037 - 6010 - 30 blister pack of 30
The blister packs consist of aluminum/aluminum Child Resistant Control (CRC) blisters.
Storage and handling
Store at controlled room temperature 20-25°C (68-77°F). Protect from light and moisture.
Last Updated: 05/2009
Edluar patient information sheet (in plain English)
Detailed Info on Signs, Symptoms, Causes, Treatments of Sleep Disorders
The information in this monograph is not intended to cover all possible uses, directions, precautions, drug interactions or adverse effects. This information is generalized and is not intended as specific medical advice. If you have questions about the medicines you are taking or would like more information, check with your doctor, pharmacist, or nurse.
back to:
~ all articles on sleeping disorders
APA Reference
Staff, H.
(2019, May 31). Edluar: Insomnia Medication (Full Prescribing Information), HealthyPlace. Retrieved
on 2026, March 3 from https://www.healthyplace.com/other-info/sleep-disorders/edluar-insomnia-medication-full-prescribing-information



