Warning: This specific article is graphic and may be triggering.)
My bulimia was a pallet of colors. As dreamy as that could sound, this wasn’t as innocent as a coloring book, rather colors were my guide.
Eating Disorders Treatment
Facing an eating disorder relapse, I’m settling into my first full day of inpatient eating disorder treatment. So in case my beating around the bush in previous posts didn’t make it clear: I’ve relapsed back into my eating disorder. I wish I could say this was uncommon. It’s not – estimates for relapse in the first year after eating disorder treatment are nearly 50%. I’ve been bouncing in and out of treatment for three years now; I have met women who have been doing so for ten years or more.
And while I could go into a long diatribe about how the eating disorder relapse rate might be lower if insurance companies covered treatment earlier in the disorder (oh wait – I’ve already done that), instead I want you to consider something. Maybe a little relapse can be good for your eating disorder recovery.
Writing an eating disorder blog, I walk a fine line. This is not my personal blog for me to whine and complain about everything that is going tough for me in recovery, and certainly not the place for me to discuss my weight, BMI, or specific behaviors. At the same time, this blog was never meant to read like a peer-reviewed journal article, sterile and clinical. There are plenty of resources out there written by professionals - which I am not - that can tell you all about the ins and outs of symptoms of eating disorders, their treatment, their recovery. In fact, there is a lot of great information in HealthyPlace's own Eating Disorder Community section.
So today, you just get a personal entry. Where I am in recovery. What I'm struggling with. What the next few weeks will bring for me.
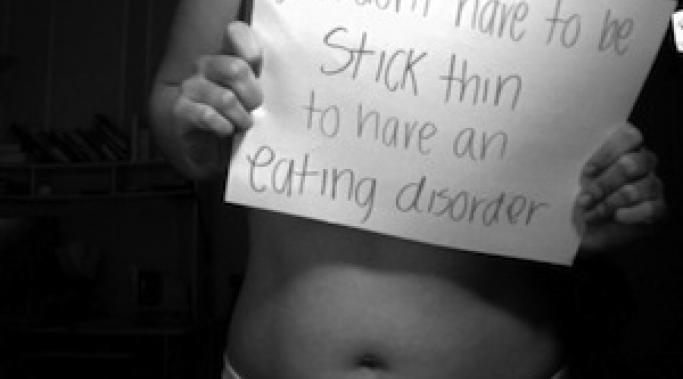
As I mentioned in my post during National Eating Disorders Awareness Week, over half of eating disorders in the United States are diagnosed as "Eating Disorder - Not Otherwise Specified" or ED-NOS. It's a tricky thing to pin down, ED-NOS is. The manifestation of this eating disorder is as varied as its many sufferers and carries a stigma and set of problems all its own.
So if I'm diagnosed with ED-NOS - what the heck does that even mean? What does it mean for my recovery? What does it mean for my access to eating disorder treatment?
One of the most frustrating things about having an eating disorder and attempting recovery is dealing with insurance companies. To be honest, I know of very few people who have had a truly positive experience with their insurance companies. This goes for all levels of eating disorder treatment: outpatient, partial hospitalization, residential, and inpatient. If you're lucky, your eating disorder treatment team will fight for you to get the insurance coverage you need. If you're not lucky, you may be doing it on your own.
While I might one day do an article later about how to deal with your insurance company and fight for the eating disorder treatment you need, today is not that day. Today's post is borne out of pure frustration.
Why Won't Insurance Companies Pay For Eating Disorder Treatment?
Open Letter to Insurance Companies
Even considering to seek inpatient treatment for your eating disorder is a big step. On the whole, we don't like to admit how bad things have gotten. Considering inpatient or residential treatment means that you have to recognize that your behaviors, your thoughts, your eating disorder is out of control. It's nearly inconceivable at some points to think this - after all, isn't your eating disorder what gives you control? Why would we seek inpatient treatment for the eating disorder?
One of the things any good therapist or dietitian will ask you when you seek treatment for your eating disorder is, “What goals do you have for our time together?”
I’ve done the treatment rodeo enough times to know that this question is coming, but I still stumble over words and fumble trying to find the “right” answer to this age-old question. To be clear, there is no “right” answer – only you can decide what things you are ready to tackle in your recovery. However, when you determine what those things are, there is a way to make effective goals that will further your recovery.
Jessica Schnaider, 41, spent eight days connected to a NG feeding tube in March. She wasn't sick. She doesn't suffer from anorexia. She isn't obese.
She merely wanted to lose weight before she got married.
To say I was incredulous would be an understatement.
I was sixteen and on the edge of puberty when I realized I hated my body. I hated having breasts, and the fact that people actually noticed them. I hated the fact that my stomach was round, my thighs were round, even my hair was too round.
I felt awkward and ugly, and that feeling plagues me to this day as I recover from anorexia.
According to The National Center of Addiction and Substance Abuse, up to one half of those with eating disorders — including anorexia, bulimia, and binge eating disorder — abuse alcohol and/or drugs. (see Eating Disorders and Addictions) This is a dangerous combination.
I didn't believe it would happen to me — until it did.